Understanding Endometriosis
15 Mar 2021|Krina Zondervan
- Research
I have long been fascinated by research into women’s health conditions, in particular benign conditions that affect many but are under-recognised and under-researched. Endometriosis is one such condition, affecting an estimated 1.6 million women in the UK alone and 190 million worldwide.
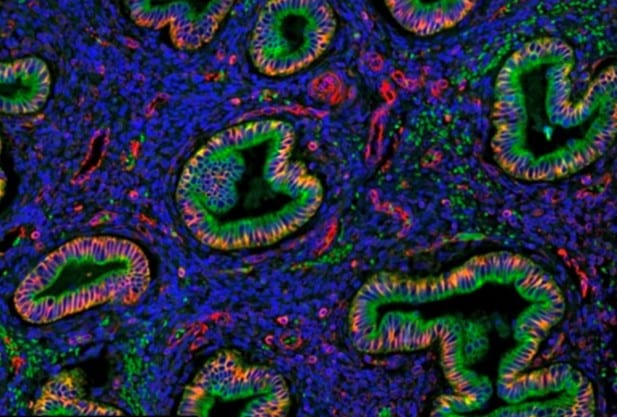
Endometriosis occurs when tissue resembling endometrium (the lining of the womb) grows outside the womb, during reproductive years. It is mainly found in the pelvis where it can be found on the ovaries, Fallopian tubes, bowel and bladder. Women commonly suffer from symptoms such as extremely painful periods, abdominal pain, painful intercourse and infertility. Having a laparoscopy (keyhole surgery) is the only way to diagnose the condition reliably. Lack of awareness of the disease and the need for surgery to establish a diagnosis has led to an average delay of 7-8 years from the start of symptoms to diagnosis among women globally. The only treatments available are hormonal treatments with many side-effects and surgical removal of disease which can be complex, often needs to be repeated, and sometimes can even result in a hysterectomy (removal of the womb).
Endometriosis is as common as asthma and type 2 diabetes, and carries a similar health care cost burden, yet it is hugely under-recognised. In a week-long feature series of articles in 2015, The Guardian highlighted that for every patient with type 2 diabetes the National Institutes of Health in the US spend about 35 dollars/year on research funding; for endometriosis this is less than 1 dollar. This is likely one of the main reasons why so little is known on what causes the disease and how best to treat it.
In 2012, Christian Becker and I established the Oxford Endometriosis CaRe Centre at the Women’s Centre, John Radcliffe Hospital, as a partnership between the University of Oxford and the Oxford University Hospitals NHS Foundation Trust and we are now one of the largest centres worldwide dedicated to researching the condition. The Centre’s mission to combine highest-quality, evidence-based patient care with cutting edge, internationally collaborative research into endometriosis.
Our research seeks to identify: 1) what causes endometriosis to help improve our understanding of its different forms; 2) non-invasive means of diagnosing the disease (e.g. biomarkers assessed through a blood test), allowing much earlier diagnosis and treatment; and 2) novel (non-hormonal) treatments and better targeting of such treatments to specific patient groups (‘stratified/personalised medicine’). To this end, the Centre’s research is highly collaborative and multidisciplinary, spanning basic science (e.g. genetics, cell biology) into the causes and characteristics of endometriosis, clinical studies investigating treatments and their effect on women, and translational research to move basic scientific findings into programmes for the development of non-invasive diagnostic tests and novel treatments, in collaboration with industry.

My own group is focused on understanding the genetics of endometriosis. We know that endometriosis can ‘run in families’. Using epidemiological and large datasets approaches, we work on identifying genetic variants that influence a woman’s risk of endometriosis, how these variants affect molecular pathways, and how environmental or ‘epigenetic’ factors influence these processes. We have just finished a study of the DNA contributed by more than 60,000 women with endometriosis, in collaboration with 24 research centres worldwide. It has provided us with a wealth of novel insights into genetic risk variants and the impact of these on specific biological pathways and subtypes of endometriosis. The data also revealed that some of the genetics involved in endometriosis is shared with other inflammatory conditions such as asthma and osteoarthritis, and other pain conditions such as migraine and back pain. This is important, because it allows us to start looking at the possibility of tweaking and repurposing treatments already available for these conditions towards endometriosis, which would greatly speed up the time needed to bring new treatments to patients.
One of the challenges we face in genetic studies of any condition is to understand what effects the genetic risk variants have in relevant tissues on downstream biology such as the expression of proteins. We have been asking women who undergo a laparascopy in our Centre to participate in our research, answer detailed questionnaires about their symptoms, and donate biological samples including blood, endometrium and endometriosis tissues. We use these to better understand the genetic effects on these tissues and the development of endometriosis both at the tissue and single-cell level.
But we cannot do this work alone! Our Centre has been promoting internationally collaborative, high quality, reproducible research through leadership of the Endometriosis Phenotyping and Biobanking Harmonisation Project (EPHect) under the auspices of the World Endometriosis Research Foundation (WERF). WERF EPHect is a global initiative that developed standardardised data and biological sample collection tools in research. These tools are already implemented in 42 centres, including Oxford Endometriosis CaRe. Our premise is that only through collaboration can we make real progress in understanding endometriosis, and ultimately provide better methods of diagnosis and treatment.
More information can be found on the Oxford Endometriosis CaRe website.

Category: Research
Author

Krina
Zondervan
Professor Krina Zondervan is Head of the Nuffield Department of Women’s and Reproductive Health and co-Director of the Oxford Endometriosis CaRe Centre. Her group focuses on understanding the genetic, molecular and environmental basis for common women’s health conditions with a large public health impact such as endometriosis.